The Effect of Antibiotics on the Gut Microbiome
The Effect of Antibiotics on the Gut Microbiome
Anti-microbial treatment adjusts the structure and extent of got microbiota species. In general, anti-infection agents diminish species' variety and incorporate the deficiency of key utilitarian taxa, bringing about shifts in digestion, expanding the vulnerability of the stomach to colonization, and the feeling of bacterial anti-toxin opposition.
The restorative or prophylaxis-utilize antimicrobial medications on the gastrointestinal microbiota cause aggravations in the microbial harmony. The degree of these changes, close by this absence of balance in the biology of the microbiota, is reliant upon the nature and pharmacokinetic profile of the medication.
What is the Gut Microbiome?
The microbiota is the assortment of microorganisms present in a specific climate. The term microbiome alludes to the climate, including the entirety of all microorganisms (microscopic organisms, eukaryotes, archaea, and infections) and their genomes and the natural circumstances present in the climate. The assortment of microscopic organisms, Archaea, eukaryotes, and infections present in the gastrointestinal lot of people is on the whole called the human stomach microbiota.
The Functional Effect of Antibiotics on the Gut
There is a reverse connection between the utilization of anti-microbials and microbial variety. In addition, the mode by which anti-microbials are conveyed applies various impacts.
Following antibacterial treatment, variety reclamation takes ~1 month; in grown-ups, rebuilding requires ~1.5 months. In grown-ups, controlling a mix of a few distinct sorts of anti-microbials (meropenem, gentamicin, and vancomycin) can build the commonness of specific types of Enterobacteriaceae close by other pathobionts with a corresponding reduction in butyrate-creating species.
Anti-microbials Alter the Balance of Microbial Species
Anti-microbials are undermining specialists that challenge the equilibrium of stomach microbial species. This disturbance in balance is appeared as diminished species variety with attendant excess of pathogenic species, known as pathobionts, for example, C difficile.
Medicines with anti-microbials are fruitful in taking out the anti-microbial helpless species. In any case, anti-toxin safe microbes commonly duplicate and have their spot. The complete microbial burden has been seen to increment following anti-toxin treatment, regardless of diminishing species variety. In an investigation of patients treated with wide range anti-toxins, the microbial burden in waste examples was expanded twofold more than seven days following treatment with B-lactams, with an expanded proportion of Bacteroidetes to Firmicute.
Additionally, the utilization of medications happens in the digestive tract because of the ownership of tremendous amounts of cytochrome P450 (CYP) compounds. These CYP compounds are dependable pick catalyzing stage one and stage two medication digestion responses. In light of oral anti-microbial treatment utilizing macrolides, changes in the gastrointestinal microbiota happen, explicitly in regards to the general overflow of bacteroids and bifidobacterium. As expressed beforehand, this delivers a specialty that obliges the development of C difficile.
Along these lines, the abuse of anti-microbials can adversely influence both the multiplication or apoptosis of digestive cells, which range from enterocytes to endocrine cells. This outcomes in the arrival of intracellular proteins, valuable markers of stomach microbiome dysregulation. In an investigation of the stomach microbiota of 1135 members, specialists tracked down an association between the microbiome and different host factors; explicitly, waste chromogranin A was related with the presence of a specific types of microorganism.
In a review led in Finland, kids somewhere in the range of two and seven years of age were dependent upon treatment with macrolides, a class of anti-toxins that incorporates erythromycin, roxithromycin, azithromycin, and clarithromycin. This treatment was related with a change in the creation of gastrointestinal verdure that continued long haul. This shift brought about a change in human stomach digestion; this was noted when kids under macrolide treatment were contrasted with a non-anti-toxin treatment bunch.
Among kids who were not presented to anti-toxins, the wealth of Collinsella, Lactobacillus, and Anaerostipes was noticed; these populaces were lower in those treated with anti-microbials. Different changes saw in microbial populaces remember a decrease for the variety and development of the microbiota north of two years. Besides, a few populaces returned quicker than others, with Bacteroides and Bifidobacterium recuperating to pre-anti-toxin status soon after macrolide organization.
Strangely, youngsters getting anti-toxins all the more habitually experienced bacterial diseases comparative with the people who didn't; this is because of the association on the interrelation of microorganisms in the stomach; the expulsion of enormous amounts of microbes brings about the general diminishment in the capability of commensal microscopic organisms.
The Impact of Antibiotics on Gut Microbiota Pre and Post Birth
The transmission of anti-microbial safe strains from mother to baby is presently understudied. In any case, it is realized that the programming of the resistant framework is firmly impacted by the microorganisms that initially colonize the stomach. This type of colonization is called vertical transmission. The upward anti-microbial safe strain move system happens during both placental and vaginal birth, through bosom milk, and move of anti-toxins in utero.
Anti-infection openness in a child companion of 12,422 showed an addition in level and weight among young men with a higher weight record. In the two sexual orientations, there was a lessening in waste bifidobacterium variety. A subsequent report involving mice model trials in which waste microbial exchange from youngsters presented to anti-microbials influenced development. This was related with a decline in thalamocortical axons, an unfortunate outgrowth of thalamic axons, and thalamocorticogenesis - this showed the way that maternal anti-toxin openness in children could unfavorably affect fetal neurodevelopment.
Hypersensitive lung irritation in posterity is additionally unequivocally connected with pre-birth anti-toxin openness. Prompted hypersensitivity is viewed as normal in neonatal resistant framework improvement as an outcome of openness to expansive range ampicillin. In these occasions, T administrative cell lack (colonic administrative T cells specifically) happens as the safe framework can't produce CD4+ T cells. Dysregulated Th1 reactions in this manner happen.
The Immunomodulatory Effects of Antibiotics on the Gut Microbiota
There is a bi-directional connection between the stomach microbiome and anti-microbials. Close by direct impacts, anti-microbials can apply roundabout impacts.
As a result of stomach microbiota dysbiosis (an interruption to the microbiota homeostasis brought about by a lopsidedness between the kinds of creatures) and dysregulation, the insusceptible framework is upset. Both in vitro and ex vivo investigations have shown the way that momentary treatment with wide range anti-microbials can influence humoral and cell safe reactions.
Likewise, a few anti-microbials have immunomodulatory impacts as well as antimicrobial action. For instance, a review has exhibited that macrolides, for example, clarithromycin can prompt in vitro and in vivo neutrophil extracellular snares (NETs). NETs are organizations of extracellular filaments, essentially made out of DNA from neutrophils, which tie microbes.
This is one of three significant techniques to battle against microorganisms; the others incorporate phagocytosis and degranulation. The NETS are additionally 'enlivened' with practical antimicrobial peptide LL-37. IL-37 can hinder the development of multidrug-safe strains and safeguard the equilibrium of the colon microbiota. The finding outlines the bidirectional impact of anti-toxins and the microbiota that hypoxia-inducible variable 1α (HIF-1α), a record factor fundamental for initiating natural safe effectors, for example, human cathelicidin IL-37, can likewise decide Candida albicans colonization opposition.
This interleukin likewise impacts wound recuperating and the upregulation of a few resistant controlled qualities. Lymphocytes are additionally receptive to IL-37 excitement because of T cell expansion, initiation, and age of administrative T cells.
The impact of anti-microbials on gastrointestinal bacterial variety and long haul misuse has likewise been recognized as a gamble factor for the improvement of metabolic problems. In an exploratory creature model, there was a relationship between's a deficiency of the stomach microbiome variety prompted by anti-microbials and expanded atherosclerosis. In particular, this was driven by a decrease in Bacteroidetes and Clostridia.
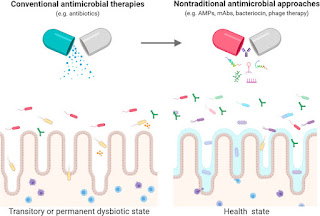
The stomach microbiota is a perplexing local area coordinated around send off organizations of metabolic interdependencies. A deep rooted group of exploration shows that stomach microbiota is indispensable for ordinary turn of events and the working of the human body. It is particularly useful in the development of the versatile resistant framework. Anti-infection agents can bring about a few unfortunate results on the stomach microbiota, from diminished variety of species, modification in metabolic movement, and the determination of anti-microbial safe organic entities, bringing about downstream impacts, for example, anti-infection related the runs and repeating C difficile diseases.
There is additionally proof that early openness to anti-toxins can affect gastrointestinal, immunological, and neurocognitive frameworks. This is hazardous because of the expanded utilization of anti-infection agents, which proposes a future expansion in the predominance of intense circumstances. To address this test, proceeding to investigate on the structure and capability of the stomach microbiota is fundamental.



Comments
Post a Comment